Vitamine und Immunabwehr
UPDATE: Eine Information der GVF zur Rolle der Mikronährstoffe für das Immunsystem (Stand 16.12.2021)
In der aktuellen Situation ist Fachwissen stärker gefragt als sonst. Die Gesellschaft für angewandte Vitaminforschung e. V. (GVF) möchte Sie unterstützen und Orientierung geben. Wir haben eine Auswahl an Publikationen von internationalen Expert*innen zum Thema Mikronährstoffe für das Immunsystem zusammengestellt.
Unser Körper ist ständig unterschiedlichsten Krankheitserregern wie Viren, Bakterien, Pilzen und Parasiten aus der Umwelt ausgesetzt. Er benötigt daher ein gut funktionierendes Abwehrsystem, um die Krankheitserreger zu bekämpfen: das Immunsystem. Dabei unterscheiden wir zwischen dem angeborenen und dem erworbenen (adaptiven) Immunsystem. Das angeborene Immunsystem reagiert in unspezifischer Weise als erste Verteidigungslinie schnell auf Pathogene. Das adaptive Immunsystem reagiert innerhalb von Tagen nach einer Infektion und baut eine spezifische Reaktion auf jeden einzelnen Erreger auf. Es stimuliert die Produktion von Immunzellen – einschließlich Antikörper – und ermöglicht es dem Körper so, die Erreger unschädlich zu machen und auf wiederholte Infektionen schützend zu reagieren.
Das Immunsystem ändert sich im Laufe des Lebens. Bei Kleinkindern ist es noch nicht vollständig entwickelt, bei Heranwachsenden reift es, sodass es bei Erwachsenen voll funktionsfähig ist. Bei älteren Menschen beginnt das Immunsystem sich wieder abzuschwächen, deshalb sind Ältere auch anfälliger für Infektionen.
Das Immunsystem benötigt eine Reihe von Mikronährstoffen – Vitamine und Mineralstoffe – für eine optimale Funktion. Dazu gehören die Vitamine A, B6, B12, C, D, E und Folat sowie die Mineralstoffe Zink, Eisen, Selen, Magnesium und Kupfer. Auch mehrfach ungesättigte Omega-3-Fettsäuren (EPA und DHA) unterstützen das Immunsystem. Eine optimale Versorgung mit diesen Mikronährstoffen stärkt die Immunfunktion und kann das Risiko, die Dauer und den Schweregrad einer Infektion reduzieren.
Die folgende Auflistung enthält Veröffentlichungen zur Rolle der Mikronährstoffe für das Immunsystem (alphabetische Reihenfolge), welche größtenteils auf den Internetseiten der Fachzeitschriften frei heruntergeladen werden können.
- Beck MA, Handy J, Levander OA (2004): Host nutritional status: the neglected virulence factor. In: Trends in Microbiology 2020; 12(9): 418-423. DOI: 10.1016/j.tim.2004.07.007.
- Berger MM, Herter-Aeberli I, Zimmermann MB et al. (2021): Strengthening the immunity of the Swiss population with micronutrients: A narrative review and call for action. In: Clinical Nutrition ESPEN. DOI: 10.1016/j.clnesp.2021.03.012.
- Broome CS, McArdle F, Kyle JAM et al. (2004): An increase in selenium intake improves immune function and poliovirus handling in adults with marginal selenium status. In: The American Journal of Clinical Nutrition 2004; 80(1): 154-162. DOI: 10.1093/ajcn/80.1.154.
- Calder PC (2012): Omega-3 polyunsaturated fatty acids and inflammatory processes: nutrition or pharmacology?. In: British Journal of Clinical Pharmacology 2012; 75(3): 645-662. DOI: 10.1111/j.1365-2125.2012.04374.x.
- Calder PC, Carr AC, Gombart AF et al. (2020): Optimal Nutritional Status for a Well-Functioning Immune System Is an Important Factor to Protect Against Viral Infections. In: Nutrients 2020; 12(4): 1181. DOI: 10.3390/nu12041181.
- Carr AC, Maggini S (2017): Vitamin C and Immune Function. In: Nutrients 2017; 9(11): 1211. DOI: 10.3390/nu9111211.
- Carr AC, Spencer E, Dixon L et al. (2020): Patients with Community Acquired Pneumonia Exhibit Depleted Vitamin C Status and Elevated Oxidative Stress. In: Nutrients 2020; 12: 1318. DOI: 10.3390/nu12051318.
- Charoenngam N, Holick MF (2020): Immunologic Effects of Vitamin D on Human Health and Disease. In: Nutrients 2020; 12: 2097. DOI: 10.3390/nu12072097.
- Gammoh NZ, Rink L (2017): Zinc in Infection and Inflammation. In: Nutrients 2017; 9(6): 624. DOI: 10.3390/nu9060624.
- Gombart AF, Pierre A, Maggini S (2020): A Review of Micronutrients and the Immune System – Working in Harmony to Reduce the Risk of Infection. In: Nutrients 2020; 12(1): 236. DOI: 10.3390/nu12010236.
- Gruber-Bzura BM (2018): Vitamin D and Influenza – Prevention or Therapy?. In: International Journal of Molecular Sciences 2018; 19: 2419. DOI: 10.3390/ijms19082419.
- Hemilä H (2017): Vitamin C and Infections. In: Nutrients 2017; 9(4): 339. DOI: 10.3390/nu9040339.
- Hemilä H, Chalker E (2013): Vitamin C for preventing and treating the common cold. In: Cochrane Database of Systematic Reviews 2013. DOI: 10.1002/14651858.CD000980.pub4.
- Ismailova A, White JH (2021): Vitamin D, infections and immunity. In: Reviews in Endocrine and Metabolic Disorders 2021. DOI: 10.1007/s11154-021-09679-5.
- Koivisto O, Hanel A, Carlberg C (2020): Key Vitamin D Target Genes with Functions in the Immune System. In: Nutrients 2020; 12: 1140. DOI: 10.3390/nu12041140.
- Maggini S, Pierre A, Calder PC (2018): Immune Function and Micronutrient Requirements Change over the Life Course. In: Nutrients 2018; 10(10): 1531. DOI: 10.3390/nu10101531.
- Mailhot G, White JH (2020): Vitamin D and Immunity in Infants and Children. In: Nutrients 2020; 12: 1233. DOI: 10.3390/nu12051233.
- Marcos A (2021): A Review of Micronutrients and the Immune System – Working in Harmony to Reduce the Risk of Infection. In: Nutrients 2021; 13: 4180. DOI: 10.3390/nu13114180.
- Martens P-J, Gysemans C, Verstuyf A et al. (2020): Vitamin D’s Effect on Immune Function. In: Nutrients 2020; 12: 1248. DOI: 10.3390/nu12051248.
- Martineau AR, Jolliffe DA, Hooper RL et al. (2017): Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. In: The BMJ 2017; 356: i6583. DOI: 10.1136/bmj.i6583.
- Pecora F, Persico F, Argentiero A et al. (2020): The Role of Micronutrients in Support of the Immune Response against Viral Infections. In: Nutrients 2020; 12: 3198. DOI: 10.3390/nu12103198.
- Rowe S, Collins PD, Stacey SE et al. (2021): Micronutrients and respiratory infections: the biological rationale and current state of clinical evaluation. In: British Journal of Hospital Medicine 2021. DOI: 10.12968/hmed.2020.0730.
- Steinbrenner H, Al-Quraishy S, Dkhil MA et al. (2015): Dietary Selenium in Adjuvant Therapy of Viral and Bacterial Infections. In: Advances in Nutrition 2015; 6(1): 73-82. DOI: 10.3945/an.114.007575.
Darüber hinaus sind in den vergangenen Wochen vermehrt Publikationen zur Bedeutung der Vitamine für die Immunabwehr im Zusammenhang mit COVID-19 erschienen. Nachfolgend sind einige dieser Veröffentlichungen aufgeführt (alphabetische Reihenfolge; kein Anspruch auf Vollständigkeit).
- Boaz M, Salem H, Navarro DA et al. (2021): Body weight, vitamin D and zinc: A review of associations with coronavirus disease (COVID-19). In: Bioactive Compounds in Health and Disease 2021; 4: 189-200. DOI: 10.31989/bchd.v4i9.839.
- Bogan-Brown K, Nkrumah-Elie Y, Ishtiaq Y et al. (2021): Potential Efficacy of Nutrient Supplements for Treatment or Prevention of COVID-19. In: Journal of Dietary Supplements 2021. DOI: 10.1080/19390211.2021.1881686.
- Butler MJ, Barrientos RM (2020): The impact of nutrition on COVID-19 susceptibility and long-term consequences. In: Brain, Behavior, and Immunity 2020; 87: 53-54. DOI: 10.1016/j.bbi.2020.04.040.
- Calder (2020): Nutrition, immunity and COVID-19. In: BMJ Nutrition, Prevention & Health 2020; 0: e000085. DOI: 10.1136/bmjnph-2020-000085.
- Carr AC (2020): A new clinical trial to test high-dose vitamin C in patients with COVID-19. In: Critical Care 2020; 24: 133. DOI: 10.1186/s13054-020-02851-4.
- Carr AC, Rowe S (2020): The Emerging Role of Vitamin C in the Prevention and Treatment of COVID-19. In: Nutrients 2020; 12: 3286. DOI: 10.3390/nu12113286.
- Carella AM, Benvenuto A, Lagattolla V et al. (2020): Vitamin supplements in the Era of SARS-CoV2 pandemic. In: GSC Biological and Pharmaceutical Sciences 2020; 11(02): 007-019. DOI: 10.30574/gscbps.2020.11.2.0114.
- Derbyshire E, Delange J (2020): COVID-19: is there a role for immunonutrition, particularly in the over 65s?. In: BMJ Nutrition, Prevention & Health 2020; 0: 1-6. DOI: 10.1136/bmjnph-2020-000071.
- Dofferhoff ASM, Piscaer I, Schurgers LJ et al. (2020): Reduced Vitamin K Status as a Potentially Modifiable Risk Factor of Severe Coronavirus Disease 2019. In: Clinical Infectious Diseases 2020. DOI: 10.1093/cid/ciaa1258.
- Galli F, Reglero G, Bartolini D et al. (2020): Better prepare for the next one. Lifestyle lessons from the COVID-19 pandemic. In: PharmaNutrition 2020; 12: 100193. DOI: 10.1016/j.phanu.2020.100193.
- Gasmi A, Tippairote T, Mujawdiya PK et al. (2020): Micronutrients as immunomodulatory tools for COVID-19 management. In: Clinical Immunology 2021; 220: 108545. DOI: 10.1016/j.clim.2020.108545.
- Gröber U (2020): COVID-19-Update für Senioren: Die Anti-SARS-CoV-2-Eigenschaften ausgewählter Mikronährstoffe. In: Zeitschrift für Orthomolekulare Medizin 2020; 18(04): 5-14. DOI: 10.1055/a-1305-4231.
- Hemilä H, de Man AME (2021): Vitamin C and COVID-19. In: Frontiers in Medicine 2021; 7: 559811. DOI: 10.3389/fmed.2020.559811.
- Holford P, Carr AC, Jovic TH et al. (2020): Vitamin C – An Adjunctive Therapy for Respiratory Infection, Sepsis and COVID-19. In: Nutrients 2020; 12: 3760. DOI: 10.3390/nu12123760.
- Janssen R, Visser MPJ, Dofferhoff ASM et al. (2020): Vitamin K metabolism as the potential missing link between lung damage and thromboembolism in Covid-19. In: British Journal of Nutrition 2020. DOI: 10.1017/S0007114520003979.
- Junaid K, Ejaz H, Abdalla AE et al. (2020): Effective Immune Functions of Micronutrients against SARS-CoV-2. In: Nutrients 2020; 12: 2992. DOI: 10.3390/nu12102992.
- Keflie TS, Biesalski HK (2020): Micronutrients and bioactive substances: Their potential roles in combating COVID-19. In: Nutrition 2020; 84: 111103. DOI: 10.1016/j.nut.2020.111103.
- Kumrungsee T, Zhang P, Chartkul M et al. (2020): Potential Role of Vitamin B6 in Ameliorating the Severity of COVID-19 and Its Complications. In: Frontiers in Nutrition 2020; 7: 562051. DOI: 10.3389/fnut.2020.562051.
- Linneberg A, Kampmann FB, Israelsen SB et al. (2021): The Association of Low Vitamin K Status with Mortality in a Cohort of 138 Hospitalized Patients with COVID-19. In: Nutrients 2021; 13(6): 1985. DOI: 10.3390/nu13061985.
- Mathers JC (2021): Nutrition and COVID-19. In: British Journal of Nutrition 2021. DOI: 10.1017/S0007114521003305.
- McAuliffe S, Ray S, Fallon E et al. (2020): Dietary micronutrients in the wake of COVID-19: an appraisal of evidence with a focus on high-risk groups and preventative healthcare. In: BMJ Nutrition, Prevention & Health 2020; 0. DOI: 10.1136/bmjnph-2020-000100.
- Michienzi SM, Badowski ME (2020): Can vitamins and/or supplements provide hope against coronavirus?. In: Drugs in Context 2020; 9: 5-7. DOI: 10.7573/dic.2020-5-7.
- Moghaddam A, Heller RA, Sun Q et al. (2020): Selenium Deficiency Is Associated with Mortality Risk from COVID-19. In: Nutrients 2020; 12: 2098. DOI: 10.3390/nu12072098.
- Naja F, Hamadeh R (2020): Nutrition amid the COVID-19 pandemic: a multi-level framework for action. In: European Journal of Clinical Nutrition 2020; 74: 1117. DOI: 10.1038/s41430-020-0634-3.
- Rayman MP, Calder PC (2021): Optimising COVID-19 vaccine efficacy by ensuring nutritional adequacy. In: British Journal of Nutrition 2021. DOI: 10.1017/S0007114521000386.
- Sabico S, Enani MA, Sheshah E et al. (2021): Effects of a 2-Week 5000 IU versus 1000 IU Vitamin D3 Supplementation on Recovery of Symptoms in Patients with Mild to Moderate Covid-19: A Randomized Clinical Trial. In: Nutrients 2021; 13: 2170. DOI: 10.3390/nu13072170.
- Samad N, Dutta S, Sodunke TE et al. (2021): Fat-Soluble Vitamins and the Current Global Pandemic of COVID-19: Evidence-Based Efficacy from Literature Review. In: Journal of Inflammation Research 2021; 14: 2091. DOI: 10.2147/JIR.S307333.
- Sarohan AR, Kızıl M, İnkaya AÇ et al. (2021): A novel hypothesis for COVID-19 pathogenesis: Retinol depletion and retinoid signaling disorder. In: Cellular Signalling 2021; 87: 110121. DOI: 10.1016/j.cellsig.2021.110121.
- Tan CW, Ho LP, Kalimuddin S et al. (2020): Cohort study to evaluate the effect of vitamin D, magnesium, and vitamin B12 in combination on progression to severe outcomes in older patients with coronavirus (COVID-19). In: Nutrition 2020; 79-80: 111017. DOI: 10.1016/j.nut.2020.111017.
- Vollbracht C, Kraft K (2021): Feasibility of Vitamin C in the Treatment of Post Viral Fatigue with Focus on Long COVID, Based on a Systematic Review of IV Vitamin C on Fatigue. In: Nutrients 2021; 13: 1154. DOI: 10.3390/nu13041154.
- Wee AKH (2020): COVID-19’s toll on the elderly and those with diabetes mellitus - Is vitamin B12 deficiency and accomplice?. In: Medical Hypotheses 2020. DOI: 10.1016/j.mehy.2020.110374.
- Zabetakis I, Lordan R, Norton C et al. (2020): COVID-19: The Inflammation Link and the Role of Nutrition in Potential Mitigation. In: Nutrients 2020; 12: 1466. DOI: 10.3390/nu12051466.
- Zhang L, Liu Y (2020): Potential interventions for novel coronavirus in China: A systematic review. In: Journal of Medical Virology 2020; 92(5): 479-490. DOI: 10.1002/jmv.25707.
Ein Teil der Publikationen zur Bedeutung der Vitamine für die Immunabwehr im Zusammenhang mit COVID-19 bezieht sich auf Vitamin D. Nachfolgend sind einige dieser Veröffentlichungen aufgeführt (alphabetische Reihenfolge; kein Anspruch auf Vollständigkeit).
- Abdrabbo M, Birch CM, Brandt M et al. (2021): Vitamin D and COVID-19: A review on the role of vitamin D in preventing and reducing the severity of COVID-19 infection. In: Protein Science 2021; 30(11): 2206. DOI: 10.1002/pro.4190.
- Alcala-Diaz JF, Limia-Perez L, Gomez-Huelgas R et al. (2021): Calcifediol Treatment and Hospital Mortality Due to COVID-19: A Cohort Study. In: Nutrients 2021; 13: 1760. DOI: 10.3390/nu13061760.
- Annweiler C, Cao Z, Sabatier J-M (2020): Point of view: Should COVID-19 patients be supplemented with vitamin D?. In: Maturitas 2020; 140: 24-26. DOI: 10.1016/j.maturitas.2020.06.003.
- Annweiler G, Corvaisier M, Gautier J et al. (2020): Vitamin D Supplementation Associated to Better Survival in Hospitalized Frail Elderly COVID-19 Patients: The GERIA-COVID Quasi-Experimental Study. In: Nutrients 2020; 12: 3377. DOI: 10.3390/nu12113377.
- Avolio AD, Avataneo V, Manca A et al. (2020): 25-Hydroxyvitamin D Concentrations Are Lower in Patients with Positive PCR for SARS-CoV-2. In: Nutrients 2020; 12: 1359. DOI: 10.3390/nu12051359.
- Aygun H (2020): Vitamin D can prevent COVID-19 infection-induced multiple organ damage. In: Naunyn-Schmiedeberg’s Archives of Pharmacology 2020. DOI: 10.1007/s00210-020-01911-4.
- Biesalski HK (2020): Vitamin D deficiency and co-morbidities in COVID-19 patients – A fatal relationship?. In: NFS Journal 2020; 20: 10-21. DOI: 10.1016/j.nfs.2020.06.001.
- Boaz M, Salem H, Navarro DA et al. (2021): Body weight, vitamin D and zinc: A review of associations with coronavirus disease (COVID-19). In: Bioactive Compounds in Health and Disease 2021; 4: 189-200. DOI: 10.31989/bchd.v4i9.839.
- Borsche L, Glauner B, von Mendel J (2021): COVID-19 Mortality Risk Correlates Inversely with Vitamin D3 Status, and a Mortality Rate Close to Zero Could Theoretically Be Achieved at 50 ng/mL 25(OH)D3: Results of a Systematic Review and Meta-Analysis. In: Nutrients 13, 3596. DOI: 10.3390/nu13103596.
- Brenner H (2021): Vitamin D Supplementation to Prevent COVID-19 Infections and Deaths – Accumulating Evidence from Epidemiological and Intervention Studies Calls for Immediate Action. In: Nutrients 2021; 13: 411. DOI: 10.3390/nu13020411.
- Chillon TS, Demircan K, Heller RA et al. (2021): Relationship between Vitamin D Status and Antibody Response to COVID-19 mRNA Vaccination in Healthy Adults. In: Biomedicines 2021; 9: 1714. DOI: 10.3390/biomedicines9111714.
- Crafa A, Cannarella R, Condorelli RA et al. (2021): Influence of 25-hydroxy-cholecalciferol levels on SARS-CoV-2 infection and COVID-19 severity: A systematic review and meta-analysis. In: EClinicalMedicine 2021; 37: 100967. DOI: 10.1016/j.eclinm.2021.100967.
- Daneshkhah A, Agrawal V, Eshein A et al. (2020): Evidence for possible association of vitamin D status with cytokine storm and unregulated inflammation in COVID‑19 patients. In: Aging Clinical and Experimental Research 2020; 32: 2141. DOI: 10.1007/s40520-020-01677-y.
- Dramé M, Cofais C, Hentzien M et al. (2021): Relation between Vitamin D and COVID-19 in Aged People: A Systematic Review. In: Nutrients 2021; 13: 1339. DOI: 10.3390/nu13041339.
- Gallelli L, Mannino GC, Luciani F et al. (2021): Vitamin D Serum Levels in Subjects Tested for SARS-CoV-2: What Are the Differences among Acute, Healed, and Negative COVID-19 Patients? A Multicenter Real-Practice Study. In: Nutrients 2021; 13: 3932. DOI: 10.3390/nu13113932.
- Ghelani D, Alesi S, Mousa A (2021): Vitamin D and COVID-19: An Overview of Recent Evidence. In: International Journal of Molecular Sciences 2021; 22: 10559. DOI: 10.3390/ijms221910559.
- Gönen MS, Alaylıoğlu M, Durcan E et al. (2021): Rapid and Effective Vitamin D Supplementation May Present Better Clinical Outcomes in COVID-19 (SARS-CoV-2) Patients by Altering Serum INOS1, IL1B, IFNg, Cathelicidin-LL37, and ICAM1. In: Nutrients 2021; 13: 4047. DOI: 10.3390/nu13114047.
- Grant WB, Lahore H, McDonnell SL et al. (2020): Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths. In: Nutrients 2020; 12(4): 988. DOI: 10.3390/nu12040988.
- Griffin G, Hewison M, Hopkin J et al. (2020): Preventing vitamin D deficiency during the COVID-19 pandemic: UK definitions of vitamin D sufficiency and recommended supplement dose are set too low. In: Clinical Medicine 2020; 21(1): 1. DOI: 10.7861/clinmed.2020-0858.
- Inserra F, Tajer C, Antonietti L et al. (2021): Vitamin D supplementation: An alternative to enhance the effectiveness of vaccines against SARS-CoV-2?. In: Vaccine 2021. DOI: 10.1016/j.vaccine.2021.07.031.
- Ish P, Agrawal S, Gupta N (2020): Vitamin C(ovi)D; An unexplored option!. In: Le Infezioni in Medicina 2020; Suppl. 1: 122-125.
- Kara M, Ekiz T, Ricci V et al. (2020): „Scientific Strabismus“ or Two Related Pandemics: COVID-19 & Vitamin D Deficiency. In: British Journal of Nutrition 2020. DOI: 10.1017/S0007114520001749.
- McCartney DM, O‘Shea PM, Faul JL et al. (2020): Vitamin D and SARS-CoV-2 infection – evolution of evidence supporting clinical practice and policy development. A position statement from the Covit-D Consortium. In: Irish Journal of Medical Science 2021; 190: 1253. DOI: 10.1007/s11845-020-02427-9.
- Mercola J, Grant WB, Wagner CL (2020): Evidence Regarding Vitamin D and Risk of COVID-19 and Its Severity. In: Nutrients 2020; 12: 3361. DOI: 10.3390/nu12113361.
- Merzon E, Tworowski D, Gorohovski A et al. (2020): Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study. In: The FEBS Journal 2020. DOI: 10.1111/febs.15495.
- Mitchell F (2020): Vitamin-D and COVID-19: do deficient risk a poorer outcome?. In: Lancet Diabetes Endocrinology 2020. DOI: 10.1016/S2213-8587(20)30183-2.
- Oscanoa TJ, Amado J, Vidal X et al. (2021): The relationship between the severity and mortality of SARSCoV-2 infection and 25-hydroxyvitamin D concentration – a metaanalysis. In: Advances in Respiratory Medicine 2021; 89: 145-157. DOI: 10.5603/ARM.a2021.0037.
- Rhodes JM, Subramanian S, Laird E et al. (2020): Perspective: Vitamin D deficiency and COVID-19 severity – plausibly linked by latitude, ethnicity, impacts on cytokines, ACE2 and thrombosis. In: Journal of Internal Medicine 2020. DOI: 10.1111/joim.13149.
- Rubin R (2021): Sorting Out Whether Vitamin D Deficiency Raises COVID-19 Risk. In: JAMA 2021. DOI: 10.1001/jama.2020.24127.
- Stroehlein JK, Wallqvist J, Iannizzi C et al. (2021): Vitamin D supplementation for the treatment of COVID-19: a living systematic review (Review). In: Cochrane Database of Systematic Reviews 2021; 5: CD015043. DOI: 10.1002/14651858.CD015043.
- Taha R, Abureesh S, Alghamdi S et al. (2021): The Relationship Between Vitamin D and Infections Including COVID-19: Any Hopes?. In: International Journal of General Medicine 2021; 14: 3849. DOI: 10.2147/IJGM.S317421.
- Tramontana F, Napoli N, El-Hajj Fuleihan G et al. (2020): The D-side of COVID-19: muscoloskeletal benefits of vitamin D and beyond. In: Endocrine 2020. DOI: 10.1007/s12020-020-02407-0.
- Vassiliou AG, Jahaj E, Pratikaki M et al. (2020): Low 25-Hydroxyvitamin D Levels on Admission to the Intensive Care Unit May Predispose COVID-19 Pneumonia Patients to a Higher 28-Day Mortality Risk: A Pilot Study on a Greek ICU Cohort. In: Nutrients 2020; 12: 3773. DOI: 10.3390/nu12123773.
- Zwart SR, Smith SM (2020): Vitamin D and COVID-19: Lessons from Spaceflight Analogs. In: The Journal of Nutrition 2020. DOI: 10.1093/jn/nxaa233.
Zur Zeit laufen in verschiedenen Ländern Studien, in denen Vitamine und andere Naturprodukte unter ärztlicher Behandlung bei COVID-19 Erkrankung therapeutisch getestet werden. Informationen über aktuelle Studien sind verfügbar unter ClinicalTrials.gov (z.B. Suche nach Studien zu Vitamin D und COVID-19 mit den Begriffen „COVID-19“ und „Vitamin D“).
Die GVF informiert regelmäßig über die Rolle der Vitamine, Carotinoide, sekundärer Pflanzenstoffe und mehrfach ungesättigter Fettsäuren für die Gesundheit. Diese Übersicht dient ausschließlich der Information und stellt keine Werbung für Vitaminprodukte und Nahrungsergänzungsmittel dar.
Fulda, Dezember 2021
UPDATE: Eine Information der GVF zur Rolle der Mikronährstoffe für das Immunsystem (Stand 16.12.2021)
The Role of Nutrition in the Immune System: Should we pay more attention? Part I of II
A guest contribution by Breda Gavin-Smith, Global Public Health Nutrition Manager, Sight and Life Foundation
As the coronavirus (COVID-19) is spreading rapidly across the globe, it is important to take note of the approaches that can help prevent and fight infections, particularly viral infections. Evidence already suggests that viral infections are one of the world's greatest public health challenges (WHO, 2020). The World Health Organization (WHO) estimates seasonal influenza results in 3-5 million cases annually. Today we understand hygiene and social distancing play a key role in protecting yourself and others from contracting a virus while also slowing the spread of infections. Here are a few simple ways to reduce your risk to infections:
- Wash your hands regularly for 20 seconds with soap and water or alcohol-based hand rub.
- Cover your nose and mouth when you sneeze or cough with a disposable tissue or flexed elbow.
- Avoid close contact with people who are sick.
- Stay at home and self-isolate from others if you feel unwell.
Incorporating Nutrition
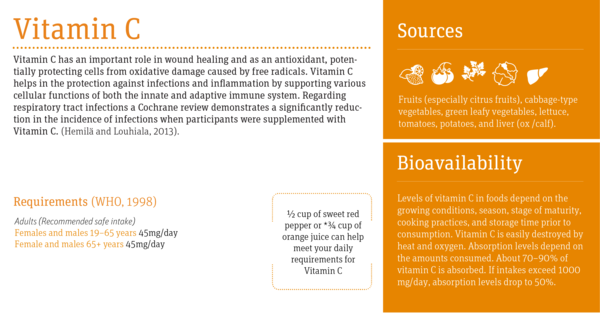
Good nutrition is fundamental to improving immunity. The immune system is the body's defense against disease and infection and it has long been established that several factors influence the function of the immune system including stress, sleep and nutrition (Song et al, 2019; Patel et al 2012 and Gombart et al 2020). The WHO guidance on diet, especially during the current pandemic states that "good nutrition is crucial for health, particularly in times when the immune system might need to fight back" (WHO, 2020). Providing a diet high in nutritious foods rich in vitamins and minerals supports optimal function of the immune system by providing antioxidants to slow damage of cells caused by free radicals (Lobo 2010) or assisting in T-cell production (Cohen 2017).
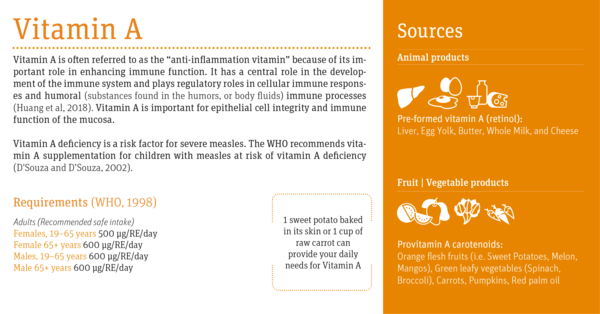
Although, presently, we do not have data concerning nutritional factors in relation to the risk and severity of viral diseases such as COVID-19 the role of nutrition in immunity has been well established. For example, a study on the role of vitamin A in the treatment of measles in children found a reduced risk of mortality and pneumonia when vitamin A was administered over two days (D'Souza and D'Souza, 2002). The European Journal of Clinical Nutrition concluded that "Without adequate nutrition, the immune system is clearly deprived of the components needed to generate an effective immune response" (Marcos et al, 2003). Good nutrition is thus important in supporting an optimum immune system which can reduce the risk of viral infections (Beck and Levander, 2000).
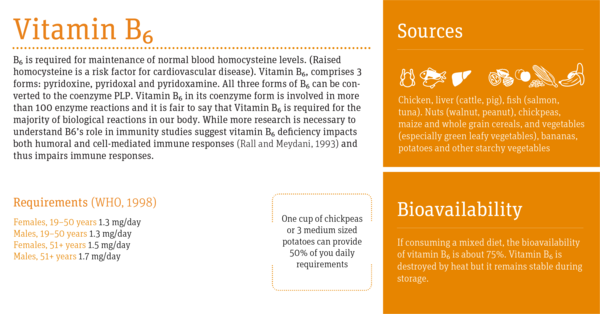
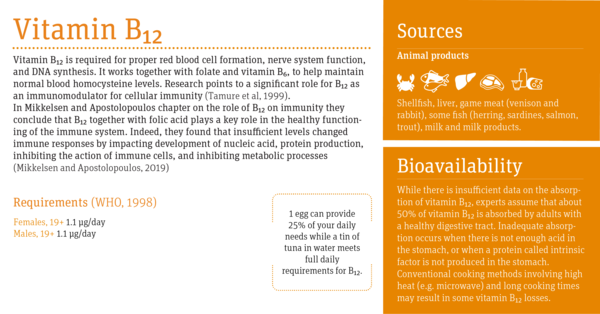
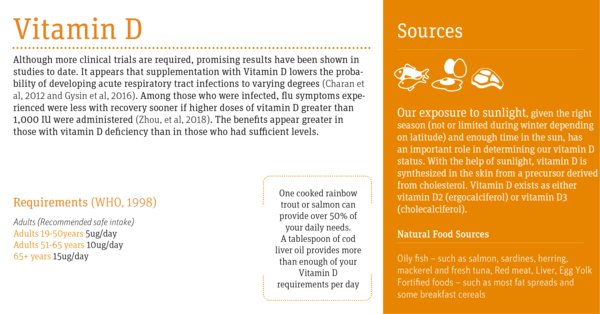
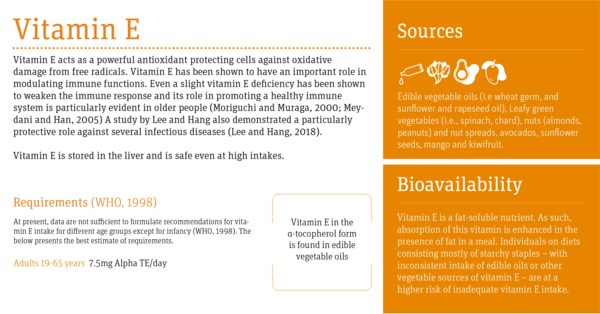
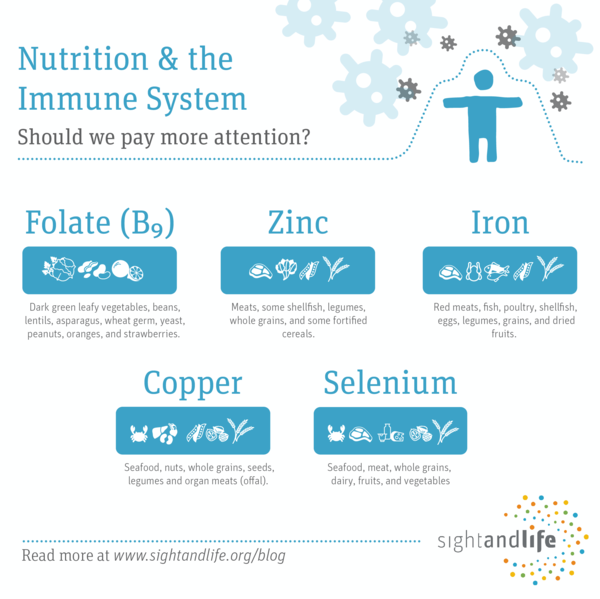
It is now recognized that the complex, integrated immune system requires several micronutrients that have essential, often synergistic roles at every phase of the immune response (Gombart et al, 2020). In fact, even marginal deficiencies in certain nutrients have been shown to impair the immune system (Gombart et al, 2020). Micronutrients are believed to work collectively to support an optimum immune system. Based on a variety of systematic and clinical data, vitamins A, B6, B12, C, D, E, folate, zinc, iron, copper, and selenium (read our Vitamin and Mineral: a brief guide) are particularly important to boosting immune response.
The chart below identifies the role of these vitamins in immunity and shares recommended amounts and sources in the diet. In a forthcoming post, we will highlight the important minerals supporting the immune system and the work Sight and Life has achieved over the past 30 years to ensure access to vital nutrients, especially for children and women of childbearing age.
*Current advice on supplementation concludes that consuming a balanced diet provides all the necessary nutrition required but where there are challenges in meeting dietary recommendations, supplements are a useful addition in helping meet our nutritional needs (EUFIC, 2020).
*Please note these are approximate values and can vary based on recommended reference values employed.
Visit the original article at https://sightandlife.org/blog/nutrition-immunity/.
References
Beck,MA and Levander, OA (2000) Host Nutritional Status and Its Effect on a Viral Pathogen The Journal of Infectious Diseases, Volume 182, Issue Supplement_1, Pages S93-S96 [Online] Available at: https://academic.oup.com/jid/article/182/Supplement_1/S93/2191642) (Accessed on 1st April 2020)
Cohen S, Danzaki K, MacIver NJ. Nutritional effects on T-cell immunometabolism. Eur J Immunol. 2017;47(2):225-235. doi:10.1002/eji.201646423
Charan, J; Goyal JP; Saxena, D and Yadav, P (2012) Vitamin D for prevention of respiratory tract infections: A systematic review and meta-analysis. J Pharmacol Pharmacother.3(4): 300-303. [Online] Available at: http://www.jpharmacol.com/article.asp?issn=0976-500X;year=2012;volume=3;issue=4;spage=300;epage=303;aulast=Charan (Accessed on 30th March 2020)
D'Souza RM and D'Souza R(2002). Vitamin A for treating measles in children. Cochrane Database Syst Rev.(1) [Online] Available at: https://www.ncbi.nlm.nih.gov/pubmed/11869601 (Accessed on 8th April 2020)
EUFIC (2020) Food and coronavirus (COVID-19): what you need to know [Online] Available at: https://www.eufic.org/en/page/food-and-coronavirus-covid-19-what-you-need-to-know (Accessed on 2nd April 2020)
Gombart AF; Pierre A and Maggini S (2020). A Review of Micronutrients and the Immune System-Working in Harmony to Reduce the Risk of Infection. Nutrients, Vol 12 (1) [Online] Available at: https://www.ncbi.nlm.nih.gov/pubmed/31963293. (Accessed on 29th March 2020)
Gysin DV, Dao D, Gysin CM, Lytvyn L, Loeb M (2016). Effect of vitamin D3 supplementation on respiratory tract infections in healthy individuals: a systematic review and meta-analysis of randomized controlled trials. PloS one.11(9).[Online] Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5025082/ (Accessed on 1st April 2020)
Hemilä H, Louhiala P (2013). Vitamin C for preventing and treating pneumonia. Cochrane database of systematic reviews (Issue 8) [Online] Available at: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD005532.pub3/abstract (Accessed 2nd April 2020)
Song, H Fall,K; Fang,F; Erlendsdóttir,H; Lu, D; Mataix-Cols, D; Fernández de la Cruz, L; D'Onofrio; BM; Gottfreðsson,M; Almqvist, C; Unnur A Valdimarsdóttir (2019) Stress related disorders and subsequent risk of life threatening infections: population based sibling controlled cohort study. BMJ 367: l5784 [Online] Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6812608/ (Accessed of 7th April 2020)
Charan, J; Goyal JP; Saxena, D and Yadav, P (2012) Vitamin D for prevention of respiratory tract infections: A systematic review and meta-analysis. J Pharmacol Pharmacother.3(4): 300-303. [Online] Available at: http://www.jpharmacol.com/article.asp?issn=0976-500X;year=2012;volume=3;issue=4;spage=300;epage=303;aulast=Charan (Accessed on 30thMarch 2020)
Lee, GY and Nim Han, S (2018) The role of Vitamin E in Immunity. Nutrients 10(11): 1614 [Online] Available at :https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6266234/ (Accessed on 2nd April 2020)
Lobo V, Patil A, Phatak A, Chandra N. Free radicals, antioxidants and functional foods: Impact on human health. Pharmacogn Rev. 2010;4(8):118-126. doi:10.4103/0973-7847.70902
Marcos, A., Nova, E. & Montero, A (2003). Changes in the immune system are conditioned by nutrition. Eur J Clinical Nutrition 57, S66-S69 [Online] Available at: https://www.nature.com/articles/1601819 (Accessed on 7th April 2020)
Meydani SN1, Han SN, Wu D. Vitamin E and immune response in the aged: molecular mechanisms and clinical implications. Immunol Rev.205pp:269-84.[Online] Available at: https://www.ncbi.nlm.nih.gov/pubmed/15882360 (Accessed on 8th April 2020)
Mikkelsen K., Apostolopoulos V. (2019) Vitamin B12, Folic Acid, and the Immune System. In: Mahmoudi M., Rezaei N. (eds) Nutrition and Immunity. Springer, ChamMoriguchi S and Muraga M (2000) Vitamin E and immunity. Vitam Horm.(Vol 59) pp:305-36 [Online] Available at: https://www.ncbi.nlm.nih.gov/pubmed/10714244 (Accessed on 1stApril 2020)
Patel SR, Malhotra A, Gao X, Hu FB, Neuman MI, Fawzi WW (2012) A prospective study of sleep duration and pneumonia risk in women. Sleep1;35(1):97-101 [Online] Available at: https://www.ncbi.nlm.nih.gov/pubmed/22215923 (Accessed on 8th April 2020)
Rall LC and Meydani SN (1993) Vitamin B6 and immune competence. Nutr Rev. Vol 51(8):217-25 [Online] Available at: https://www.ncbi.nlm.nih.gov/pubmed/8302491 (Accessed on 2nd April 2020)
Tamure; J; Kubota,K; Murakami H; Sawamura, M; Matsushima T; T;Tamura, Saitoh, T; Kurabayshi, H and Naruse, T(1999) Immunomodulation by vitamin B12: augmentation of CD8+ T lymphocytes and natural killer (NK) cell activity in vitamin B12-deficient patients by methyl-B12 treatment Clin Exp Immunol Vol 116(1): 28-32.[Online] Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1905232/ (Accessed on 13th April 2020)
WHO (2020) Food and Nutrition tips during self-quarantine [Online] Available at: www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/novel-coronavirus-2019-ncov-technical-guidance/food-and-nutrition-tips-during-self-quarantine (Accessed on 2nd April 2019)
World Health Organization (2020) WHO launches new global influenza strategy [Online] Available at: https://www.who.int/news-room/detail/11-03-2019-who-launches-new-global-influenza-strategy (Accessed on April 7th2020)
WHO (1998) Vitamin and mineral requirements in human nutrition Second edition. https://apps.who.int/iris/bitstream/handle/10665/42716/9241546123.pdf?ua=1
Zhiyi Huang;Yu Liu;Guangying Qi; David Brand and Song Guo Zheng (2018) Role of Vitamin A in the Immune System. J Clin Med 7(9): 258. [Online] Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6162863/ (Accessed on 28th March 2020)
Zhou, Jian MD*; Du, Juan MD*; Huang, Leting MD†; Wang, Youcheng MD‡; Shi, Yimei MD‡; Lin, Hailong MD(2018) Preventive Effects of Vitamin D on Seasonal Influenza A in Infants - A Multicenter, Randomized, Open, Controlled Clinical Trial The Pediatric Infectious Disease Journal Vol 37 (8) pp 749-754 [Online] https://journals.lww.com/pidj/fulltext/2018/08000/Preventive_Effects_of_Vitamin_D_on_Seasonal.5.aspx (Accessed on 2nd April 2011)
The Role of Nutrition in the Immune System: Should we pay more attention? Part II of II
A guest contribution by Breda Gavin-Smith, Global Public Health Nutrition Manager, Sight and Life Foundation
Vitamins and minerals, known as micronutrients, are nutrients needed by our body for optimal function and often required in only small amounts. These micronutrients are not produced in the body and thus must be obtained from our food (CDC, 2020). Micronutrient deficiencies can have devastating outcomes. At least half of children globally under 5 experience vitamin and mineral deficiencies (UNICEF, 2020) and globally 2 million people suffer "hidden hunger". Micronutrient deficiency is often referred to as "hidden hunger" because they develop slowly over time and their impact is often invisible until permanent damage has been done (UNICEF, 2020).
Is food a solution?
A recent article published in the Sight and Life Magazine concluded that nutrient requirements were not met in diets with high stable food consumption as is the case in many low- and middle-income countries (Depford et al, 2019). Many approaches have been adopted with the aim of eliminating micronutrient deficiencies including periodic vitamin A supplementation, iodized salt, targeted iron/folate supplementation, fortified flour, other fortified foods, home fortification with micronutrient powders, and homestead food production. Efforts continue globally to find approaches supporting the eradication of hidden hunger because of the impact deficiencies have on health and survival (Semba, 2012). During times of emergency, as we are currently experiencing with the coronavirus (COVID-19) pandemic, nutrition is of greater importance in order to ensure our immune system operation is optimized to fight such infections.
What to consider?
In The Role of Nutrition in Immunity: Should we pay more attention? Part 1 of II, we considered the research demonstrating the central role nutrition plays in effective functioning of our immune system. As surmised by Wu and colleagues, "There is little argument that deficiency in both macronutrients and micronutrients causes immune function impairment, which can be reversed by nutrient repletion" (Wu et al, 2019). Also highlighted was the World Health Organization's (WHO) guidance on the importance of a healthy diet during the current pandemic where it states the crucial role of nutrition for health, particularly in times when the immune system might need to fight back such as is the case during COVID-19 (WHO, 2020). Included in the review was the current research and thinking on the factors that impact our immune system's ability to fight infection focusing specially on the role of micronutrients. Gombart and colleagues concluded that indeed the complex, integrated immune system requires several micronutrients that have essential, often synergistic roles at every phase of the immune response (Gombart et al, 2020) with even marginal deficiencies impacting our immune response. Based on a variety of systematic and clinical data, vitamins A, B6, B12, C, D, E, and minerals copper, folate, iron, selenium, and zinc (read our Vitamin and Mineral: a brief guide) are particularly important to boosting immune response and we looked specifically at the research supporting the role of vitamins in the immune response. If you have not read Part I already, the blog post can be found here.
In this blog we will look specially at folate and the trace minerals thought to have a significant role in the immune system and examine if research backs up these claims.
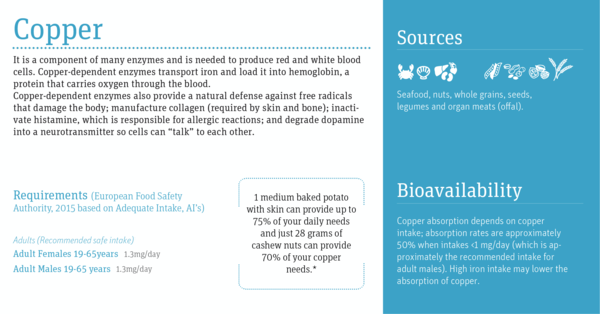
Copper
After iron and zinc, copper is the most abundant dietary trace mineral. It is a component of many enzymes and is needed to produce red and white blood cells. Copper-dependent enzymes transport iron and load it into hemoglobin, a protein that carries oxygen through the blood.
Copper-dependent enzymes also provide a natural defense against free radicals that damage the body; manufacture collagen (required by skin and bone); inactivate histamine, which is responsible for allergic reactions; and degrade dopamine into a neurotransmitter so cells can "talk" to each other.
In a study by Djoko and colleagues they concluded that copper was essential for effective innate immune response and inadequate levels leads to increased susceptibility to bacterial infection (Djoko et al, 2015). Understanding coppers influence on these positive impacts requires further research.
Current advice on supplementation concludes that consuming a balanced diet provides all the necessary nutrition required but where there are challenges in meeting dietary recommendations, supplements are a useful addition in helping meet our nutritional needs (EUFIC, 2020).
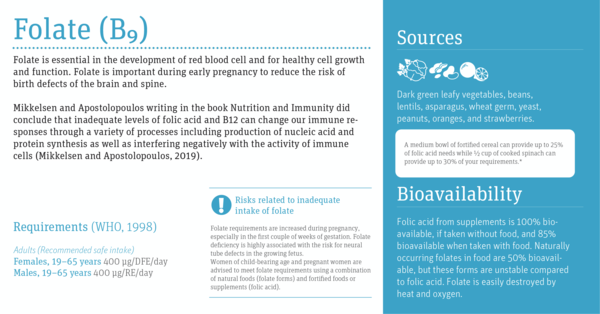
Folate (B9)
Folate works together with vitamin B12 to form healthy red blood cells. It is also necessary for normal cell division, the normal structure of the nervous system and specifically in the development of the neural tube (which develops into the spinal cord and skull) in the embryo. Vitamins B6, B12, and folate are involved with maintenance of normal blood homocysteine levels.
While its role in DNA synthesis points to immunity, Dhur and colleagues found that cell-mediated immunity is particularly impacted by inadequate folate status (Dhur et al, 1991). More studies are required to confirm these findings. Mikkelsen and Apostolopoulos writing in the book Nutrition and Immunity did conclude that inadequate levels of folic acid and B12 can change our immune responses through a variety of processes including production of nucleic acid and protein synthesis as well as interfering negatively with the activity of immune cells (Mikkelsen and Apostolopoulos, 2019).
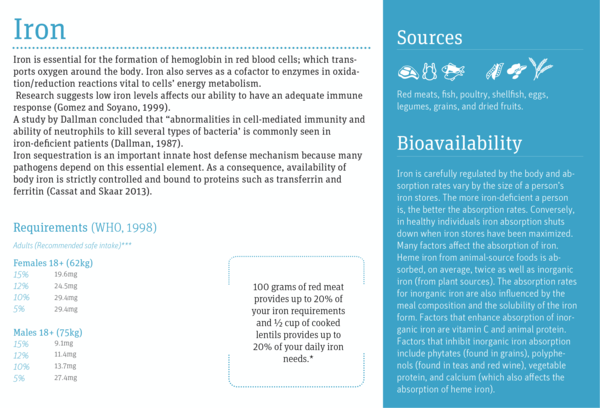
Iron
Iron is essential for the formation of hemoglobin in red blood cells; which transports oxygen around the body. Iron also serves as a cofactor to enzymes in oxidation/reduction reactions (i.e., accepts or donates electrons). These reactions are vital to cells' energy metabolism.
Research suggests low iron levels affects our ability to have an adequate immune response (Gomez and Soyano, 1999). It is required for immune cell production and growth particularly lymphocytes, which are related to the initiation of specific responses to infection (Gomez and Soyaon, 1999).
A study by Dallman concluded that "abnormalities in cell-mediated immunity and ability of neutrophils to kill several types of bacteria" is commonly seen in iron-deficient patients (Dallman, 1987).
Iron sequestration is an important innate host defense mechanism because many pathogens depend on this essential element. As a consequence, availability of body iron is strictly controlled and bound to proteins such as transferrin and ferritin (Cassat and Skaar 2013).
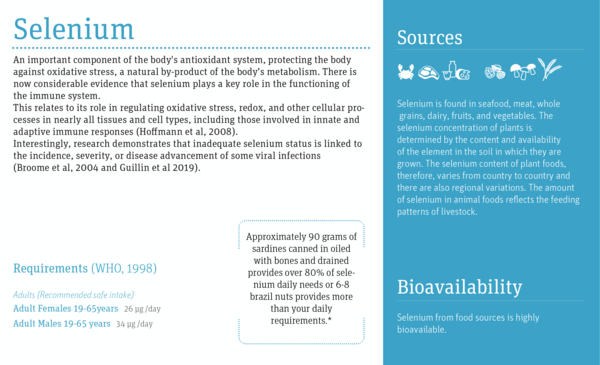
Selenium
Selenium is an important component of the body's antioxidant system, protecting the body against oxidative stress, a natural by-product of the body's metabolism. There is now considerable evidence that selenium plays a key role in the functioning of the immune system.
This relates to its role in regulating oxidative stress, redox, and other cellular processes in nearly all tissues and cell types, including those involved in innate and adaptive immune responses (Hoffmann et al, 2008).
Interestingly research demonstrates that inadequate selenium status is linked to the incidence, severity, or disease advancement of some viral infections (Broome et al, 2004 and Guillin et al 2019); Arthur and colleagues when examining selenium and immunity concluded that deficiency can result in the creation of proinflammatory compounds that would influence risk toward diseases such as heart disease and cancer (Arthur et al, 2003).
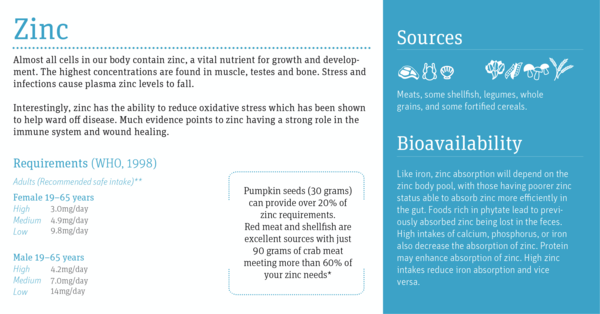
Zinc
Almost all cells in our body contain zinc, a vital nutrient for growth and development. The highest concentrations are found in muscle, testes and bone. The body tightly regulates zinc levels. Stress and infections for example cause plasma zinc levels to fall. Zinc has a key role as a catalyst in a wide range of reactions and a large number of enzymes. A study by Maret suggests this and he concluded that the human genome encodes up to 3,000 zinc proteins.
Much evidence points to zinc having a strong role in the immune system and wound healing. Research shows that zinc affects multiple elements of the immune system, from the barrier of the skin to gene regulation within lymphocytes (Shankar and Prasad, 1998). Maywald and colleagues reported that both zinc insufficiency as well as excess leads to changes in immune cell numbers and activities, which results in increased susceptibility to infections and development of inflammatory diseases (Maywald et al, 2017). Interestingly, zinc has the ability to reduce oxidative stress which has been shown to help ward off disease.
*Please note these are approximate values and can vary based on recommended reference values employed.
**Criteria for establishing zinc requirements are based on categorizing diets as high, medium and low bioavailability of zinc. For detailed information please refer to WHO Requirements 1998.
***Iron requirements fluctuate throughout the life course. Iron needs increase during menstruation, pregnancy, and periods of rapid growth such as early childhood and adolescence. Recommended levels are based on bioavailability of iron from certain diets and vary from 15 % bioavailability to 5 %.
Visit the original article at https://sightandlife.org/blog/nutrition-immunity-part-ii/.
References
Arthur, JR; McKenzie, RC and Beckett, GJ (2003) Selenium in the Immune System, The Journal of Nutrition, Vol 133 (5), pp:1457S-1459S [Online] Available at: https://academic.oup.com/jn/article/133/5/1457S/4558526 (Accessed on 15th April 2020)
Broome, Broome CS; McArdle, F; Kyle, JAM; Andrews, F; Lowe, NM; Hart, CA; Arthur, JR and Jackson,MJ (2004) An increase in selenium intake improves immune function and poliovirus handling in adults with marginal selenium status. The American Journal of Clinical Nutrition, Vol 80 (1), pp:154-162 [Online] Available at: https://academic.oup.com/ajcn/article/80/1/154/4690273 (Accessed on 17th April 2020)
Cassat JE, Skaar EP (2013). Iron in infection and immunity. Cell Host Microbe. 13(5) pp:509-519. [Online] Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3676888/ (Accessed on 21st April 2020)
CDC (2020) Micronutrient Facts. [Online] Available at: https://www.cdc.gov/nutrition/micronutrient-malnutrition/micronutrients/index.html (Accessed on 20th April 2020)
Dallman, PR (1987) Iron Deficiency and the Immune Response Am J Clin Nutr 46(2):329-34.[Online] Available at: https://pubmed.ncbi.nlm.nih.gov/3303900/ (Accessed on 18th April 2020)
Depford, A; Baldi,G; Bose,I; Badham, J; Knight, F;Klemm, and dePee, S (2019) Requirements not Met by Diets High in Staple Foods [Online] Available at: https://sightandlife.org/wp-content/uploads/2018/12/SALMZ_0218-1.pdf (Accessed on 21st April 2020)
Dhur, A and Galan, P and Hercberg, S (1991) Folate Status and the Immune System Prog Food Nutr Sci 15(1-2):43-60.[Online] Available at: https://pubmed.ncbi.nlm.nih.gov/1887065/ (Accessed on 17th April 2020)
Djoko, KY; Ong, CL Y; Walker, MJ and McEwan, AG (2015) The Role of Copper and Zinc Toxicity in Innate Immune Defense against Bacterial Pathogens J Biol Chem 290(31): pp18954-18961 [Online] Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4521016/ (Accessed on 18th April 2020)
EFSA (2015) Scientific Opinion on Dietary Reference Values for copper. [Online] Available at: https://www.efsa.europa.eu/en/efsajournal/pub/4253 (Accessed on 18th April 2020)
Gombart AF; Pierre A and Maggini S (2020). A Review of Micronutrients and the Immune System-Working in Harmony to Reduce the Risk of Infection. Nutrients, Vol 12 (1) [Online] Available at: https://www.ncbi.nlm.nih.gov/pubmed/31963293 (Accessed on 29thMarch 2020)
Guillin, O.M.; Vindry, C.; Ohlmann, T.; Chavatte, L (2019) Selenium, Selenoproteins and Viral Infection Nutrients2019, 11(9), 2101 [Online] Available at: https://www.ncbi.nlm.nih.gov/pubmed/31487871 (Accessed on 21st April 2020)
Hoffmann, PR and Marla J. Berry, MJ (2008) The influence of selenium on immune responses. Mol Nutr Food Res; 52(11): 1273-1280. [Online] Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3723386/ (Accessed on 15th April 2020)
Maret W (2013) Zinc biochemistry: from a single zinc enzyme to a key element of life. Adv Nutr. 4(1)pp:82-91. [Online] Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3648744/ (Accessed on 20th April 2020)
Maywald, M; Wessels, I and Rink, L (2017) Zinc Signals and Immunity Int J Mol Sci 18(10): 2222.[Online] Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5666901/ (Accessed on 17th April 2020)
Mikkelsen K., Apostolopoulos V. (2019) Vitamin B12, Folic Acid, and the Immune System. In: Mahmoudi M., Rezaei N. (eds) Nutrition and Immunity. Springer, Cham
Shankar , AH , and AS Prasad (1998) Zinc and Immune Function: The Biological Basis of Altered Resistance to Infection Am J Clin Nut 68(2 Suppl):447S-463S. [Online] Available at: https://pubmed.ncbi.nlm.nih.gov/9701160/ (Accessed on 17th April 2020)
Soyano, A and M Gómez M (2008) Role of Iron in Immunity and Its Relation With Infections Arch Latinoam Nutr 49(3 Suppl 2):40S-46S [Online] Available at: https://pubmed.ncbi.nlm.nih.gov/10971835/ (Accessed on 15th April 2020)
Semba RD (2012). The historical evolution of thought regarding multiple micronutrient nutrition. J Nutr 142(1):pp:143S-56S. [Online]Available at: https://pubmed.ncbi.nlm.nih.gov/22157539/ (Accessed on 20th April 2020)
UNICEF (2020) Micronutrients [Online] Available at: https://www.unicef.org/nutrition/index_iodine.html (Accessed on 20th April 2020)
World Health Organization (2020) Food and Nutrition tips during self-quarantine [Online] Available at: http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/novel-coronavirus-2019-ncov-technical-guidance/food-and-nutrition-tips-during-self-quarantine (Accessed on 2nd April 2019)
World Health Organization (2020) WHO launches new global influenza strategy [Online] Available at: https://www.who.int/news-room/detail/11-03-2019-who-launches-new-global-influenza-strategy (Accessed on April 7th 2020)
WHO (1998) Vitamin and mineral requirements in human nutrition Second edition. https://apps.who.int/iris/bitstream/handle/10665/42716/9241546123.pdf?ua=1
Wu D; Lewis E D., Pae M and Meydani Simin N (2019) Nutritional Modulation of Immune Function: Analysis of Evidence, Mechanisms, and Clinical Relevance Frontiers in Immunology Vol 9 pp 31-60 [Online] Available at: https://www.frontiersin.org/articles/10.3389/fimmu.2018.03160/full (Accessed on 17th April 2020)